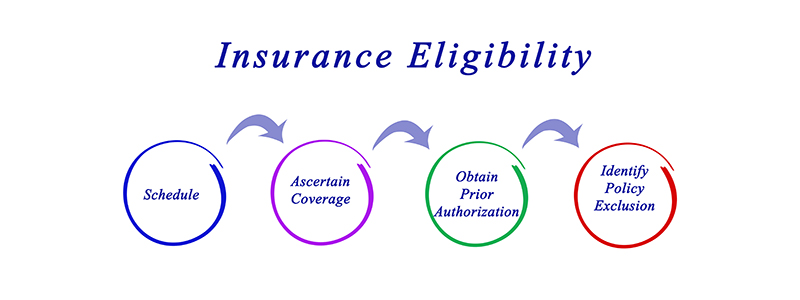
We are proficient in interpreting and applying the intricacies of health plans and policy changes. We facilitate real-time verification of insurance coverage and process versification. Our dusk-to-dawn approach ensures that you start each day with accurate and updated insurance information. Our experts, equipped with efficient insurance eligibility verification systems, aim to optimize your revenue cycle, minimize claim denials, and ensure swift reimbursements. To enhance the financial stability and operational efficiency of your healthcare practice, connect with us today.